The landscape of modern medicine is shifting under our feet. For decades, the medical community viewed chronic pain as an unfortunate, lingering symptom of physical injury. However, recent scientific breakthroughs in early 2026 have fundamentally redefined our understanding. We now know that chronic pain is not just a symptom but a distinct neurological condition. Most importantly, researchers have identified that silencing a specific brain circuit can actually prevent and reverse chronic pain entirely.
- The Landmark 2026 Discovery: The CGIC Pathway
- Understanding the Mechanism of Brain Circuit Silencing
- The Survival Switch: Y1 Receptor Neurons
- Genetic Breakthroughs: The SLC45A4 Gene and Pain Sensitivity
- Advanced Therapeutic Interventions in 2026
- 1. Non-Invasive Brain Stimulation (rTMS and tDCS)
- 2. Brain-Machine Interfaces (BMI)
- 3. Chemogenetics and Designer Drugs
- The End of the Opioid Era
- Live Daily Information: Updates for January 28, 2026
- Frequently Asked Questions (FAQ)
- Can chronic pain really be reversed?
- Is silencing a brain circuit safe?
- How soon will these treatments be available to the public?
- What is the difference between acute and chronic pain?
- Conclusion and Research Sources
This discovery marks a pivotal moment for over 1.5 billion people worldwide who suffer from persistent pain. By moving away from systemic medications and focusing on the precision of neural pathways, we are entering an era where pain can be “switched off” at its source.
The Landmark 2026 Discovery: The CGIC Pathway
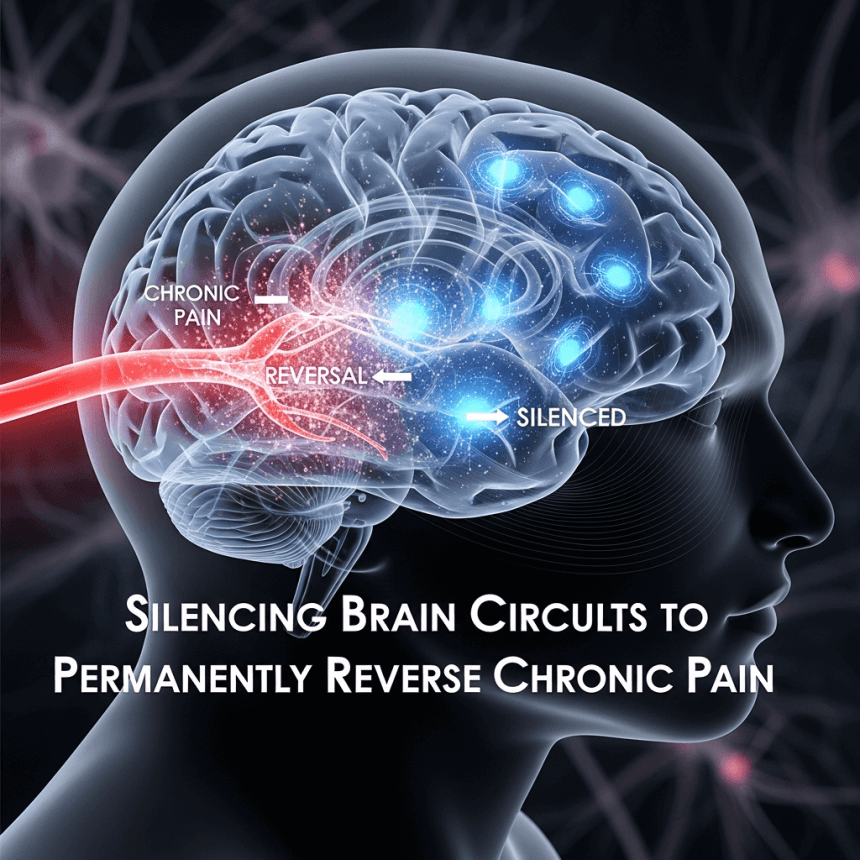
In a groundbreaking study released in January 2026, researchers at the University of Colorado Boulder identified a specific neural circuit hidden within the caudal granular insular cortex (CGIC). This understudied region of the brain appears to be the “master switch” for the transition from acute to chronic pain.
According to Dr. Linda Watkins, a distinguished professor of behavioral neuroscience, the CGIC plays a minimal role in processing immediate or acute pain. Its primary function is a “decision-maker.” It determines whether a pain signal should persist long after the initial injury has healed. The study, published in the Journal of Neuroscience, demonstrates that if this circuit is silenced during the early stages of an injury, chronic pain never develops. Even more impressively, if the pain is already established, silencing this pathway can cause the chronic pain to effectively melt away.
The research utilized state of the art chemogenetic tools to manipulate precise populations of neurons. By observing how these cells signal the somatosensory cortex and the spinal cord, scientists found that an overactive CGIC keeps the body in a state of high alert, causing even a light touch to be perceived as painful (a condition known as allodynia).
Understanding the Mechanism of Brain Circuit Silencing
To understand how silencing a brain circuit works, we must first understand the concept of neuroplasticity. The brain is not a static organ; it constantly rewires itself based on experience. Chronic pain is essentially a “maladaptive” form of neuroplasticity. The brain learns to be in pain, strengthening the neural pathways that carry pain signals until they fire automatically.
Silencing the circuit involves disrupting this feedback loop. In preclinical models, scientists use techniques like optogenetics (using light to control neurons) or chemogenetics (using engineered receptors that respond to specific designer drugs). For human applications in 2026, the focus has shifted toward non-invasive neuromodulation and advanced brain-machine interfaces.
The Role of the Caudal Granular Insular Cortex (CGIC)
The CGIC is a sugar-cube-sized cluster of cells tucked deep within the folds of the insula. Human neuroimaging has long shown that chronic pain patients exhibit hyper-activity in this region. The 2026 CU Boulder study confirms that the CGIC acts as a relay station. It receives signals of distress and instructs the spinal cord to remain in a sensitized state. When we “silence” this circuit, we are essentially telling the brain to “reset” its pain threshold to normal levels.
The Survival Switch: Y1 Receptor Neurons
While the CGIC handles the persistence of pain, another critical discovery from late 2025 involves the lateral parabrachial nucleus (lPBN) in the brainstem. Researchers at the University of Pennsylvania identified a group of neurons known as Y1 receptor-expressing neurons.
These neurons act as a biological priority system. They process pain, but they also respond to more urgent survival needs like hunger, thirst, or fear. This explains why an injured animal can still run from a predator without feeling the full weight of its pain. The brain has a built-in “override switch.”
By targeting these Y1R neurons with neuropeptide Y (NPY), scientists can dampen ongoing pain signals. This “tonic activity” (the persistent idling of pain neurons) can be quieted, providing a roadmap for new pharmacological treatments that mimic the body’s natural survival-based pain suppression.
Genetic Breakthroughs: The SLC45A4 Gene and Pain Sensitivity

Adding to the complexity of pain management is the recent identification of the SLC45A4 gene. In a massive collaborative study involving the University of Oxford and the UK Biobank, researchers found that variants in this gene significantly impact an individual’s susceptibility to chronic pain.
The SLC45A4 gene encodes a neuronal polyamine transporter. Polyamines are natural chemicals that regulate how nerves respond to stimuli. When polyamine levels are too high, nerve cells become over-sensitized, leading to long-term damage and persistent pain signals.
Identifying this genetic link allows for a more personalized approach to pain management. In the future, a simple genetic test could identify patients at high risk of developing chronic pain after surgery, allowing doctors to intervene by silencing the relevant brain circuits before the pain becomes entrenched.
Advanced Therapeutic Interventions in 2026
The transition from laboratory discovery to clinical application is moving faster than ever. Several high-tech interventions are currently being tested or deployed to target these specific brain circuits.
1. Non-Invasive Brain Stimulation (rTMS and tDCS)
Repetitive Transcranial Magnetic Stimulation (rTMS) and Transcranial Direct Current Stimulation (tDCS) are leading the charge in non-drug therapies. By applying magnetic or electrical pulses to specific areas like the prefrontal cortex or the insula, doctors can “down-regulate” the activity of overactive pain circuits.
New data from early 2026 suggests that a five-day course of preventative rTMS before a major surgery can significantly reduce the risk of the patient developing post-operative chronic pain. This “pre-habilitation” for the brain is set to become a standard of care in surgical centers.
2. Brain-Machine Interfaces (BMI)
Startups like Neuralink and other neurotech firms are exploring the use of implanted or wearable brain-machine interfaces. These devices can monitor neural activity in real-time. When they detect the signature firing pattern of the CGIC or lPBN pain circuits, they can deliver a precise micro-pulse to silence the activity before the patient even feels the sensation of pain.
3. Chemogenetics and Designer Drugs
The development of “designer receptors exclusively activated by designer drugs” (DREADDs) is the holy grail of precision medicine. While still largely in the clinical trial phase, the goal is to use gene therapy to place these receptors in the specific brain circuits responsible for pain. A patient would then take a pill that only affects those specific neurons, leaving the rest of the brain and body untouched. This would eliminate the systemic side effects and addiction risks associated with traditional painkillers.
The End of the Opioid Era
The most significant impact of silencing brain circuits is the potential to end the reliance on opioids. Traditional pain medications work by flooding the entire nervous system with chemicals that dampen all signals, leading to sedation, constipation, and a high risk of dependency.
By contrast, targeting a specific brain circuit is a “sniper” approach rather than a “carpet bomb.” It addresses the neurological root of the pain without affecting the reward centers of the brain or the respiratory system. This shift represents the most promising path forward in resolving the global opioid crisis while still providing effective relief for those in genuine need.
Live Daily Information: Updates for January 28, 2026
As of today, January 28, 2026, several clinical trials have opened for enrollment regarding the tKIWI system, a personalized tDCS device designed to target the insular cortex for neuropathic pain relief. Additionally, the University of California San Francisco (UCSF) has just announced a new cohort for their “Closed-Loop Deep Brain Stimulation” study, focusing on patients with treatment-resistant chronic back pain.
Researchers are closely watching the results of a Phase II trial by Veralox Therapeutics, which is testing a compound that blocks the enzyme system responsible for “locking” neurons into a chronic pain state. If successful, this could be the first disease-modifying analgesic to hit the market.
Frequently Asked Questions (FAQ)
Can chronic pain really be reversed?
Yes. Latest research from 2026 suggests that by silencing the specific brain circuits (like the CGIC) that maintain the pain state, the nervous system can be “reset,” effectively reversing chronic conditions that have lasted for years.
Is silencing a brain circuit safe?
Techniques like rTMS and tDCS are non-invasive and have been shown to be exceptionally safe with minimal side effects. More invasive methods like brain-machine interfaces or gene therapy are currently reserved for the most severe, treatment-resistant cases under strict clinical supervision.
How soon will these treatments be available to the public?
Non-invasive stimulation therapies are already available in many specialized clinics. More advanced “circuit-specific” drugs and gene therapies are currently in Phase II and Phase III clinical trials, with expected wider availability within the next 2 to 5 years.
What is the difference between acute and chronic pain?
Acute pain is a vital warning signal of immediate tissue damage. Chronic pain is when the brain’s “warning system” gets stuck in the “on” position, continuing to signal danger even after the initial injury has healed.
Conclusion and Research Sources
The discovery that we can silence specific brain circuits to prevent and reverse chronic pain is a monumental leap in medical science. It offers a future where pain is no longer a life sentence but a manageable neurological setting. As we continue to map the intricate highways of the human brain, the hope for a pain-free life becomes a tangible reality for millions.