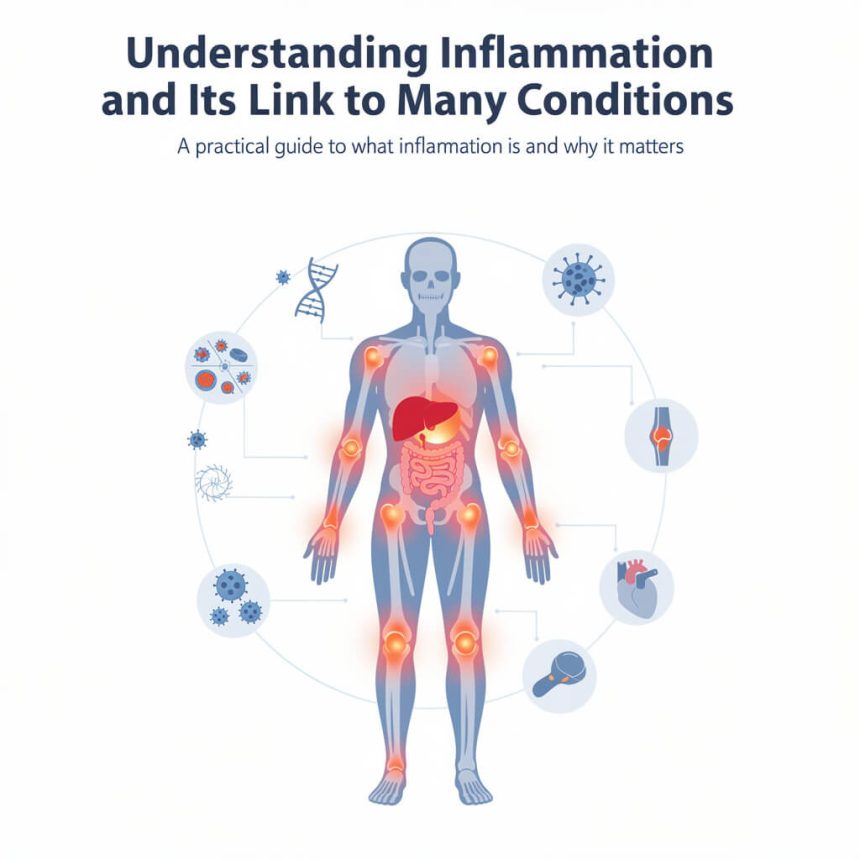
In the evolving landscape of modern medicine, specifically as we enter the early days of 2026, the scientific community has reached a consensus on a singular, powerful phenomenon that underlies nearly every major chronic health challenge. This phenomenon is inflammation. While once viewed merely as a localized reaction to a bee sting or a sprained ankle, we now understand that systemic, low grade inflammation is the invisible driver behind everything from metabolic syndrome to neurological decline. As a top health writer and researcher, I have spent years tracking the progression of immunological studies, and the insights emerging this January are more transformative than ever before. To truly master your health in this new era, you must understand how this biological fire is ignited, how it spreads, and most importantly, how it can be extinguished through precision science and intentional living.
- The Dual Nature of the Inflammatory Response
- Current Medical Breakthroughs: Live Updates for January 2026
- The Molecular Markers: How We Measure Inflammation Today
- Inflammation and Cardiovascular Health: The Endothelial Connection
- Neurological Implications: The Brain on Fire
- Autoimmune Conditions and the Loss of Tolerance
- The Gut-Immune Axis: The Ground Zero of Inflammation
- Metabolic Syndrome and the Role of Adipose Tissue
- Anti-Inflammatory Lifestyle: The Foundations of Resilience
- The Importance of Sleep and Stress Management
- Future Horizons: What to Expect Next
- Conclusion
The Dual Nature of the Inflammatory Response
To understand the complexity of inflammation, one must first recognize its dual role as both a protector and a potential destroyer. Inflammation is a fundamental survival mechanism. When the body encounters a pathogen, such as a virus or bacteria, or experiences physical trauma, the innate immune system orchestrates a complex cascade of events. Blood vessels dilate to allow white blood cells to reach the site of injury, and chemical signaling molecules called cytokines are released to coordinate the defense. This is acute inflammation. It is loud, visible, and essential for healing. Without it, even a minor cut could become life threatening.
However, the modern medical crisis revolves around chronic inflammation. This occurs when the “off switch” for the immune response fails to engage. In these cases, the body remains in a persistent state of high alert. Instead of a targeted strike against a specific invader, the immune system begins a slow, smoldering attack on the body’s own tissues. This persistent activation is often referred to as “low grade” because it does not cause the immediate pain or swelling associated with an injury. Instead, it works quietly in the background, damaging DNA, degrading cellular membranes, and disrupting delicate hormonal balances over decades.
Current Medical Breakthroughs: Live Updates for January 2026
As of January 5, 2026, several groundbreaking studies have redefined our approach to inflammatory management. A major study released earlier this morning in Nature Medicine highlights a significant discovery regarding environmental triggers. Researchers have identified that dozens of widely used industrial chemicals, previously thought to be biologically inert, are actually damaging beneficial gut bacteria and inducing systemic inflammation. This study underscores the fact that our modern environment is a constant source of immune provocation.
Furthermore, on January 3, 2026, researchers at the University of Toronto announced the discovery of a new biomarker for multiple sclerosis (MS) progression. They found that a specific ratio of immune signals, specifically CXCL13 to BAFF, can signal “compartmentalized inflammation” within the central nervous system. This allows clinicians to identify patients who are experiencing active neurological damage before physical symptoms even worsen. This shift toward predictive diagnostics is the hallmark of 2026 medicine.
Additionally, a significant CRISPR breakthrough reported on January 1, 2026, has shown that scientists can now “turn on” anti-inflammatory genes without cutting the DNA itself. By removing chemical tags that act as molecular anchors on specific genes, this new epigenetic therapy offers a way to naturally boost the body’s internal defenses against chronic disease. These real time updates show that we are moving away from broad immunosuppressants and toward highly targeted, precision interventions.
The Molecular Markers: How We Measure Inflammation Today
In 2026, the standard blood panel has undergone a significant upgrade. We no longer rely solely on a general white blood cell count to assess health. Instead, clinicians are looking at highly specific markers of systemic stress.
The most prominent of these is high sensitivity C-reactive protein, or hs-CRP. This protein is produced by the liver in response to inflammatory cytokines like Interleukin-6 (IL-6). Unlike the standard CRP test used for acute infections, the high sensitivity version can detect the minute elevations associated with cardiovascular risk and metabolic dysfunction. A reading above 2.0 mg/L is often a signal that the silent fire is burning too brightly.
Another critical marker gaining traction this year is the Neutrophil to Lymphocyte Ratio (NLR). This simple calculation from a standard complete blood count provides a snapshot of the balance between the innate and adaptive immune systems. A high NLR is increasingly being used as a prognostic tool for everything from solid tumor progression to the severity of cardiovascular events. By monitoring these markers, individuals can take proactive steps to adjust their lifestyle before a formal diagnosis occurs.
Inflammation and Cardiovascular Health: The Endothelial Connection
Heart disease remains a leading global health challenge, but the perspective has shifted from a “plumbing” problem to an “inflammatory” problem. While cholesterol is a factor, it is the inflammation of the blood vessel lining, known as the endothelium, that truly sets the stage for disaster.
When the endothelium becomes inflamed, it becomes “sticky.” This allows lipids and immune cells to adhere to the vessel walls, forming plaques. Chronic inflammation also weakens the fibrous cap covering these plaques. If the cap ruptures, it triggers a clotting response that can lead to a heart attack or stroke. Recent research from the end of 2025 has emphasized that reducing systemic inflammation is just as important as lowering LDL cholesterol for long term heart health. This is why many cardiologists are now prescribing anti-inflammatory protocols alongside traditional lipid lowering therapies.
Neurological Implications: The Brain on Fire
One of the most concerning aspects of chronic inflammation is its impact on the brain. For a long time, the brain was thought to be “immunologically privileged,” meaning it was protected from the body’s immune fluctuations by the blood brain barrier. We now know that persistent peripheral inflammation can actually “leak” into the central nervous system.
This process is a primary driver of neurodegenerative conditions like Alzheimer’s disease and Parkinson’s. In these conditions, specialized immune cells in the brain called microglia become overactive. Instead of cleaning up debris, they begin to release neurotoxic substances that destroy healthy neurons. Furthermore, there is a growing body of evidence linking neuroinflammation to mental health. New clinical guidelines for 2026 suggest that certain cases of “treatment resistant” depression may actually be the result of a “brain on fire,” where inflammatory cytokines interfere with the production and signaling of serotonin and dopamine.
Autoimmune Conditions and the Loss of Tolerance
In autoimmune diseases like rheumatoid arthritis, Lupus, and Crohn’s disease, the inflammatory response is the primary feature of the condition. These diseases represent a total loss of “immune tolerance,” where the body can no longer distinguish between self and non self.
The latest research in 2026 is focusing on the “resolution phase” of inflammation. Most current drugs work by blocking inflammatory pathways. However, emerging therapies are aiming to stimulate the body’s natural “pro-resolving” mediators, such as resolvins and protectins. These molecules actively signal the immune system to stop the attack and begin tissue repair. This shift from “blocking” to “resolving” represents a major leap forward in managing autoimmune health without the side effects of traditional immunosuppression.
The Gut-Immune Axis: The Ground Zero of Inflammation
The gastrointestinal tract houses approximately 70 percent of the human immune system. Therefore, it is no surprise that gut health is the primary determinant of systemic inflammation. The intestinal barrier, or “gut lining,” is a single layer of cells that must decide what enters the bloodstream and what stays out.
When this barrier is compromised, a condition often called “leaky gut,” undigested food particles and bacterial toxins can slip through. The immune system reacts to these “intruders” by launching a systemic inflammatory response. Modern diets high in ultra-processed foods and low in fermentable fibers are the primary culprits in degrading the gut microbiome and the protective mucus layer. In 2026, “Microbiome Personalization” has become a top health trend, where individuals use real time stool analysis to identify which bacterial strains are driving their specific inflammatory markers.
Metabolic Syndrome and the Role of Adipose Tissue
Obesity is no longer viewed simply as a storage of excess energy. We now understand that white adipose tissue, or body fat, is an active endocrine organ. Excess fat cells, particularly those stored around the abdominal organs, secrete a constant stream of inflammatory cytokines.
This creates a vicious cycle. Inflammation leads to insulin resistance, which in turn leads to more fat storage and more inflammation. This “meta-inflammation” is the root cause of type 2 diabetes and non alcoholic fatty liver disease. Breaking this cycle requires a multi-pronged approach that goes beyond simple calorie counting. It requires specific interventions that improve insulin sensitivity and reduce the inflammatory output of fat cells.
Anti-Inflammatory Lifestyle: The Foundations of Resilience
While medical technology is advancing rapidly, the most effective tools for managing inflammation remain within our daily control. In 2026, the concept of “Exercise as Molecular Medicine” has gained mainstream scientific backing. Short, intense bursts of movement followed by adequate recovery have been shown to trigger the release of “myokines,” which are muscle-derived signaling molecules that have potent anti-inflammatory effects throughout the body.
Nutrition also plays a pivotal role. The “Anti-Inflammatory Diet” of 2026 is not a one-size-fits-all plan. It is a framework focused on high-phytonutrient density and stable blood sugar. Key components include:
- Omega-3 Fatty Acids: Found in fatty fish and algae, these are the direct precursors to pro-resolving mediators.
- Polyphenols: Compounds in berries, dark chocolate, and green tea that “dampen” inflammatory signaling pathways like NF-kB.
- Fiber-Rich Prebiotics: Foods like artichokes, leeks, and onions that feed the beneficial bacteria responsible for producing butyrate, a short-chain fatty acid that repairs the gut lining.
- Cruciferous Vegetables: Broccoli and kale contain sulforaphane, which activates the Nrf2 pathway, the body’s primary internal antioxidant and anti-inflammatory defense system.
The Importance of Sleep and Stress Management
It is impossible to discuss inflammation without addressing the nervous system. The “Stress-Inflammation Connection” is a primary focus of health research this year. When we are under chronic stress, the body releases cortisol. While cortisol is technically an anti-inflammatory hormone, chronic exposure causes immune cells to become resistant to its effects. This is known as “glucocorticoid receptor resistance,” and it essentially leaves the immune system without its primary regulator.
Furthermore, sleep is the period when the brain’s “glymphatic system” flushes out metabolic waste and inflammatory markers. Just one night of poor sleep has been shown to significantly increase levels of IL-6 the following day. In 2026, sleep optimization is no longer seen as a luxury but as a non-negotiable medical necessity for anyone looking to reduce their inflammatory load.
Future Horizons: What to Expect Next
Looking toward the remainder of 2026 and into 2027, the focus is shifting toward “biological age” testing. Instead of looking at the date on your birth certificate, doctors will use “epigenetic clocks” to measure how much inflammation has aged your cells. This allows for a much more personalized approach to longevity. We are also seeing the rise of “peptides,” short chains of amino acids that can act as highly specific signaling molecules to modulate immune function with minimal side effects.
The “inflammaging” phenomenon, where aging is driven by chronic, low grade inflammation, is finally being tackled at its source. By targeting “senescent cells” (often called “zombie cells” that refuse to die and instead secrete inflammatory signals), new therapies are showing the potential to not only slow but actually reverse some of the damage caused by decades of systemic stress.
Conclusion
Inflammation is the common thread that weaves through the tapestry of human disease. By understanding its mechanisms and staying informed about the latest research breakthroughs, you can transition from a passive observer of your health to an active participant in your wellness. The data from early 2026 is clear: the most effective way to prevent chronic disease is to keep the “silent architect” of inflammation in check through a combination of precision diagnostics, targeted nutrition, and mindful living.